Between the expanding population and the increasing number of surgical procedures being performed, demand for surgical services is climbing. One study has predicted a 14% to 47% increase in surgical demand across all surgical fields by 2020. Given the high cost of operations, an efficient workflow is paramount, and there is increasing focus on using technology to streamline processes.
At Geisinger Health System (Danville, Pennsylvania), we were using a manual scheduling process for several years. This system had many advantages, but efficiency wasn't one of them. A project to change from this manual system to an electronic one took a couple of years to implement but ultimately allowed us to increase efficiency, staff and physician satisfaction, and even patient safety. Here's how we did it.
Antiquated process
Geisinger Health System serves patients in northeast Pennsylvania, with eight hospital campuses that include 1,746 inpatient beds and 91 ORs. Geisinger Medical Center (GMC), the largest of the Geisinger hospitals, is a tertiary care Level 1 trauma center.
GMC houses a main operative suite with 37 ORs, an endoscopy suite with nine procedure rooms, an interventional radiology suite, a cardiac catheterization and electrophysiology suite, and a labor and delivery floor with two ORs. There are 13 surgical service lines.
The OR suite accommodates elective and emergent cases each weekday from 7 am to 5 pm and Saturdays from 7 am to 3 pm. Additional rooms are open 24 hours a day as needed for emergency surgeries.
The traditional method of assigning OR staff involved use of a physical wall magnet board. Secretaries hand-wrote assignments that were then transcribed onto magnetic strips and hung onto an assignment board. This process, which was used for many years, allowed staff to provide essentially limitless information by writing with a dry-erase marker. Nurses, technologists, and staff had become familiar with the board, and it gave them a quick orientation of the schedule.
Drawbacks to this method were that the information was only available at the OR control desk, requiring phone calls and pages to disseminate the information to the postanesthesia care unit (PACU), same-day surgery recovery area, and other areas of the surgical suite. Numerous phone calls between surgeons and staff were needed to know where staff were assigned.
The process also required two steps to generate the paper assignments and then transcribe them onto the magnet board. Additionally, the centrality of information created a traffic jam at the control desk at each shift change.
Attempts were made to develop an Excel spreadsheet that could be printed and allow for disseminating information beyond the OR control desk. The major disadvantage was that only one person could enter data at any given time, and it lacked autofeed capability.
The primary reason for implementing an electronic assignment board was to expedite care to patients in the pre- and postoperative care units. Assignments change frequently, resulting in multiple calls to find the assigned anesthesiologist to address patient pain control, anxiety, and questions from the patient or family.
Staff in these areas were frustrated with the ever-changing assignments and the multiple phone calls or pages. We clearly needed to change the system.
Initial steps
A multidisciplinary group including anesthesiologists, nurses, and administrative staff was established in 2012, and a timeline for meetings was developed. The group made decisions on hardware acquisition, including purchase and placement of monitors in the OR suite.
An information technology team was tapped to program and install the hardware and customize the software. Additional follow-up meetings were held to address implementation issues. The software application code was revisited after several rounds of changes to optimize it.
We considered several extensions of electronic medical record systems, but their platforms were too cumbersome to meet the basic functions needed. Eventually, the system that was developed was built on ColdFusion with jQuery for user interface components.
The application is interfaced with the staff scheduling system to narrow the list of available staff members (staff who are not working on a specific day are not selectable to be added to the schedule). The interface can be accessed at any computer connected to the Geisinger network.
The application is Web-based, which allows Geisinger to distribute to any PC via browser without an installation.
Communication logistics
The interface provides various views (OR main, PACU, break room) to customize the information displayed and make it relevant to the location (sidebar, p 27). No patient information is displayed or managed within the application.
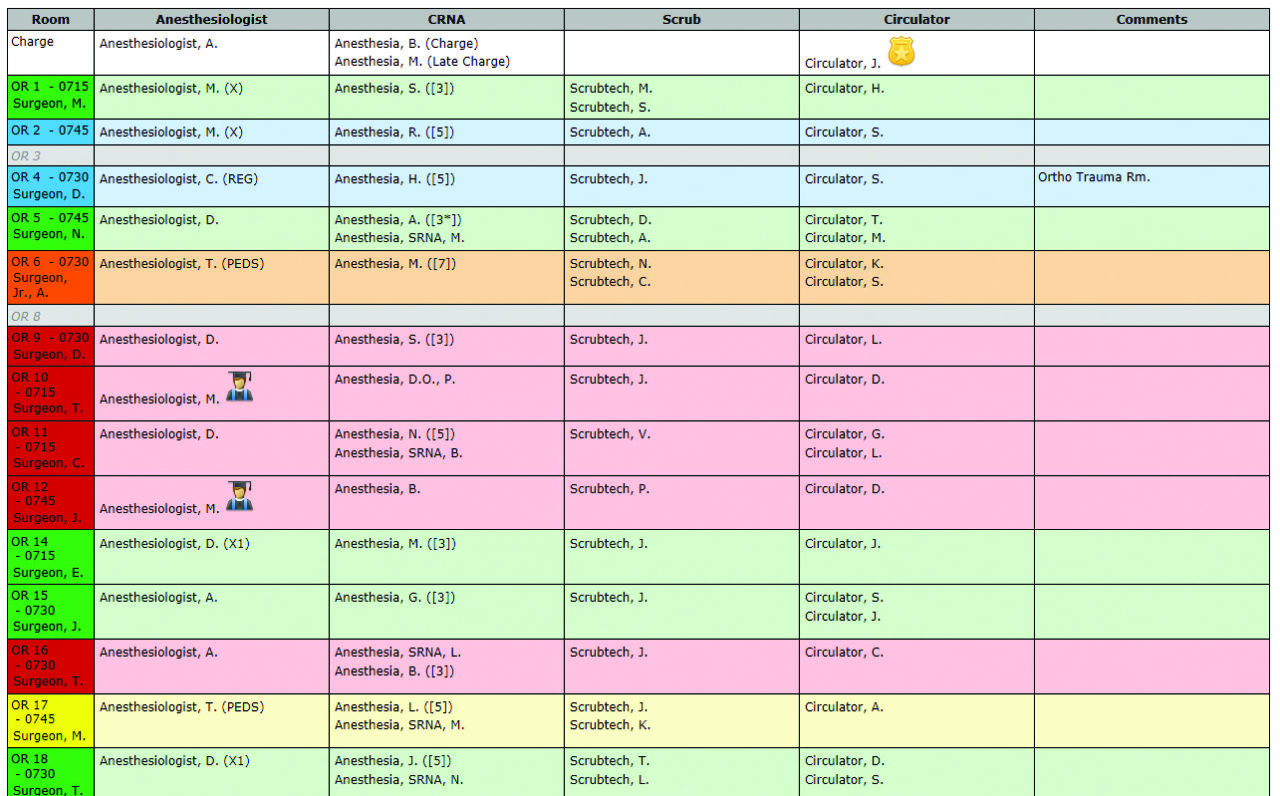
Main OR display of electronic assignment system at Geisinger Medical Center.
Source: Geisinger Medical Center. Used with permission.
Various communication options exist for assignment notification. All staff members receive an email in their employee account with their upcoming assignment. Staff can opt for additional notification via text message and/or personal email. Smart phones are provided for staff to use during the day if they do not own a device.
During the first several months of implementation, some staff were resistant to checking email or text messaging for assignments, but most users adapted to the new system without difficulty.
The advantage and convenience of receiving an assignment directly to one's email or device, and the ability to access this at any time, have far outweighed any initial resistance to the process change. Between the option of receiving a text or checking email, employees have found that at least one of those methods works well for them.
Notification arrives at 6 pm for the next day, and again at 6 am to cover changes to the schedule. Staff can see what time their room opens and which team members and surgeon they are working with. An additional module takes advantage of staff contact information to be used in case of emergencies.
Administrators in the application can send communication by individual roles (anesthesiologists, CRNAs, nursing, etc) if desired. Predefined messages are available so the entire message does not have to be authored in the middle of an emergency. Messages can be sent via text message or email, which is useful in different situations (eg, overtime shifts available vs all hands on deck).
Implementation challenges
Among the challenges to implementation were network issues, scalability (performance improvements in code), and nonstandard methods of assigning staff. Additionally, incorporating all necessary data onto one screen required several attempts. The goal was not to "electrify" the paper process, but rather to use technology to make the process better.
Some individuals had difficulty visualizing something other than the paper process. There were some features that did not work for all groups (eg, the solution for 20 anesthesiologists is not the same as the one for 200 OR nursing staff members).
Although all departments used the same scheduling system, each had different codes for vacations, etc. To address the customized practices in each department, a filter for the scheduling data was developed.
The testing process was challenging. OR responsibilities made it difficult for initial testers to truly dedicate time to utilizing and validating the system.
The data-locking feature was an initial hurdle as well. This feature was originally necessary so that users did not overwrite changes on the master schedule. However, this became a bottleneck because multiple charge persons in anesthesia and nursing needed access to change the schedule simultaneously. This problem was alleviated by locking only the data that each user had access to rather than imposing a complete lock on the entire schedule.
In addition to technical and logistical factors, some OR employees were reluctant to change the system. Implementation necessitated a small workflow change for each employee, but that has since become routine.
Rather than reporting to the control desk, staff need only to check email or text messaging for upcoming assignments. If staff are dissatisfied or want to change their assignment, they request this directly via their operations manager, in the same way they did previously.
Feedback from staff was continuously gathered by those on the multidisciplinary project team so that appropriate modifications could be made.
Results
Implementing the electronic assignment process has markedly improved overall communication in the perioperative suite. A staff member can rapidly identify and contact the appropriate CRNA, anesthesiologist, or circulating nurse with any questions or notify them when a patient is ready for the OR. Giving this information to the staff has put them in control of information and reduced phone calls and pages.
The up-to-the-minute assignment information removed the distraction of multiple phone calls to providers and/or the OR control desk (where the charge nurses make the assignment changes), thus improving care for our patients.
There has been a subsequent decrease in the amount of overhead paging. Overall, this has improved relationships between all OR personnel.
Perhaps most importantly, the communication improvements have strengthened patient safety. Nursing staff in the PACU and same-day surgery unit know who is taking care of patients, and they can more quickly reach the appropriate provider. The reduction in wait time for care in the preoperative area reduces delays and improves the patient experience.
This project was internally driven and executed by Geisinger employees with relatively small capital expense. Adopting an electronic staff assignment system not only has revolutionized the daily workflow at GMC but also continues to bridge communication gaps and enhance patient care across all groups of staff and geographic locations in our surgical suite. ✥
The authors are with Geisinger Health System, Danville, Pennsylvania: Weston Shertzer, DO, anesthesiology resident; Abdel Ragab, MD, medical director, anesthesiology; Timothy Frymoyer, associate vice president, anesthesiology; Matt Fitzpatrick, lead Web app developer; Courtney Gorgone, MBA, SSBB, administrative director, surgical suites; and Kelly Baylor, CCRC, clinical research coordinator, anesthesiology.
References
Etzioni D, Liu J, Maggard M, et al. The aging population and its impact on the surgery workforce. Ann Surg. 2003;238(2):170-177.
Lemke H. Workflow in the operating room. Biomed Technik 2005;50(5):153.
Sanberg W S, Daily B, Egan M, et al. Deliberate perioperative systems design improves operating room throughput. Anesthesiology. 2005;103(2):406-418.
